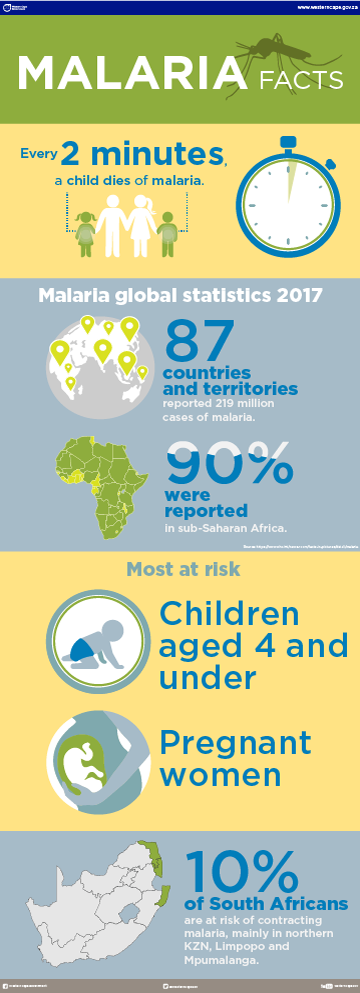
Key facts about malaria
Malaria is a mosquito-borne disease transmitted through the bite of the female Anopheles mosquito. Malaria can be cured, but it can be fatal if not treated quickly. The disease usually occurs in tropical and sub-tropical regions across the world.
The annual malaria season has started and typically, malaria infections increase in the South African summer months from September until the end of May. The high-risk areas in South Africa include:
- The far north of KwaZulu-Natal Province bordering Mozambique,
- The low-veld areas of Mpumalanga Province including the Kruger National Park but excluding Nelspruit and White River, and
- The north-eastern parts of Limpopo Province.
Take a look at the South African map of our malaria regions.
6 Key facts
- Malaria is preventable and curable.
- Early diagnosis and treatment of malaria reduces disease and prevents deaths. It also contributes to reducing malaria transmission.
- Malaria isn’t contagious and can’t be spread from person to person like a cold or the flu.
- Climate conditions influence transmission as it may affect the number and survival of mosquitoes, such as rainfall patterns, temperature and humidity.
- Your own immunity is a very important factor, especially if you live in an area of moderate or intense transmission conditions.
- Transmission is more intense in places where the vector mosquito lifespan is longer and where the females of local vector species bite several times in 1 night. A vector is any agent (person, animal, or microorganism) that carries and transmits an infectious pathogen into another living organism) – in this case it’s the mosquito.
Initiatives which combat malaria will be successful if communities are mobilised through health education to:
- Recognise the signs and symptoms of malaria.
- Provide more home-based treatment.
- Seek treatment when they become ill.
- Use personal protective measures.
Prevention
Prevention of malaria involves protecting yourself against mosquito bites and taking antimalarial medicines. But public health officials strongly recommend that young children and pregnant women avoid travelling to areas where malaria is common.
You should take a number of factors into consideration prior to travelling to an area where malaria is prevalent, these include:
- The malaria risk in the area being visited.
- The length of stay in the area.
- The time of year (in areas of seasonal malaria transmission) or time of day of the visit.
- The intensity of transmission and prevalence of drug-resistant malaria in the area.
- Pregnancy, breastfeeding, age, other diseases, immune status (including those who had have a splenectomy) and concurrent medications.
- Type of accommodation, for example, air-conditioned rooms or camping.
- Mode of travel, for example, backpacking, motoring, or flying.
- Whether the destination is rural or urban.
- Activities (safaris or jungle expeditions), especially between dusk and dawn.
- Access to medical care.
Medicines to prevent malaria
Many effective antimalarial drugs are available. Your healthcare provider will decide on the best drug for you, based on your:
- Travel plans
- Medical history
- Age
- Drug allergies
- Pregnancy status
To allow enough time for the drugs to become effective and for a pharmacy to prepare any special doses of medicine (especially doses for children and infants), visit your healthcare provider 4 to 6 weeks before travel.

Prevent mosquito bites
Apart from the obvious medications, there are other things you can do to reduce your risk of exposure, for example:
- Try to avoid being outside from dusk until dawn, malaria-carrying mosquitoes are the most active then.
- Wear long-sleeved shirts and long pants when outside.
- Use mosquito repellents and be sure to apply as instructed on the label directions.
- Stay in a room that has air-conditioning, screens on windows and doorways, and a mosquito net surrounding your bed.
- Use insect repellent spray indoors.
Signs and symptoms
Following the bite of an infected mosquito, you may remain asymptomatic for 12 to 35 days, depending on the species of malaria. This is known as the incubation period.
You should suspect malaria if you or someone you know, have an unexplained fever after visiting an area where malaria is common. The symptoms of malaria include:
- Fever
- Chills
- Sweating
- Headaches
- Body aches
- Tiredness
- Stomach problems, for example, loss of appetite, nausea and vomiting, belly pain, and diarrhoea
- Coughing
- Jaundice (skin that looks yellow)
- Fast heart rate or breathing
When malaria becomes severe, it can cause symptoms such as:
- Confusion
- Hallucinations
- Seizures
- Dark or bloody urine
Who's at risk?
Malaria can affect everyone, but those most at risk are:
- Children under 5.
- Pregnant women.
- People living in emergency situations.
- People living with HIV/AIDS.
Because the malaria parasite is found in red blood cells of an infected person, malaria is also transmitted through blood transfusion, organ transplant, or the shared use of needles or syringes contaminated with blood. Malaria may also be transmitted from a mother to her unborn infant before or during delivery (‘congenital’ malaria).
South Africa poses a rather low threat of malaria as the disease is only mildly present in the province of KwaZulu-Natal, Limpopo (including the Kruger National Park), and Mpumalanga.
 Preventing malaria during travel
Preventing malaria during travel
Do some research about the country that you’re planning to visit and find out if the area is in a high- risk malaria region. Consult with your local doctor or pharmacist if there is a high risk of contracting malaria at your intended destination. Your doctor or pharmacist will recommend the best medication for you.
Some malaria medicines take time before they become fully effective. Make sure to consult with your doctor at least 4 weeks before you travel.
For more information please visit
- Malaria No More
- World Health Organisation
- International Association for Medical Assistance to Travellers (IAMAT)
- Roll Back Malaria Project