TB and you
What is TB?
 TB is an infectious (yet curable), airborne disease that's caused by a germ that attacks and damages the lungs. It can be easily passed to others through coughing or sneezing.
TB is an infectious (yet curable), airborne disease that's caused by a germ that attacks and damages the lungs. It can be easily passed to others through coughing or sneezing.
How are people infected?
When an infected person coughs, sneezes or spits saliva onto the ground, the germs are spread into the surrounding air and remain there for a long time. If you inhale that air, you can breathe in the germs and get infected.
What are some of the factors that contribute to the weakening of the immune system?
- Poor nutrition
- Getting older
- Disease such as uncontrolled diabetes
- Physical and emotional stress
- Alcoholism
- Prolonged steroid therapy
- Cancer treatment
- Viral infections
What are the early symptoms?
| Persistent cough for more than two weeks | General feeling of illness or fever for more than two weeks | Drenching night sweats | Unexplained weight loss | Tiredness |
If not treated early TB symptoms will worsen and will include:
| Continued, severe coughing | Pain in the chest while breathing or coughing | Discoloured or bloody sputum (mucus coughed up from the lungs) | Tiredness |
| Loss of appetite | Weight loss | Drenching night sweats | Mild fever or chills |

Where and how do I get tested?
You can get free testing at your nearest clinic. Testing for adults is done by taking 2 sputum samples and the results are normally available after 2 to 3 days.
Testing for children is done using skin tests and chest X-rays.
TB treatment
TB treatment is free at clinics. TB can only be cured if the full course of treatment, which can be from 6 to 8 months, is completed. People who stop treatment are likely to develop multi-drug resistance, making the TB more difficult to cure. Treatment is in 2 phases:
The intensive phase is when 4 different drugs in tablet form are given for 5 days a week, for 2 to 3 months.
The second phase is the continuation phase, in which 2 drugs are given for 5 days a week, for 4 to 5 months.
First-time TB clients must be treated for 6 months, while clients who have had TB before must take TB medicine for 8 months. If there are side effects from the medication, the client must return to the clinic.
Children with TB are given different medicines and treated for 4 months only. To try and prevent TB, babies should be immunised with the BCG vaccine, which is available free of charge at all primary healthcare clinics.
Note: Like with any other medication, there can be side effects to TB treatment. The common side effects are rashes, nausea and vomiting. You should not stop using your medication as the side effects usually disappear after certain time.
What is MDR TB?
Multi-Drug Resistant TB (MDR TB) is a specific form of TB that does not respond to “ordinary” TB treatment. As a result it is difficult to treat and needs specialised treatment.
Eight things you should know about MDR tuberculosis
How to prevent TB
- Know the symptoms of TB and urge anyone showing TB symptoms to get tested immediately.
- Ensure that people living with TB take their full course of medication, as instructed.
- Make sure that children below the age of 5 are vaccinated with the BCG vaccine to prevent TB infection. Children younger than 5 who are in contact with a TB patient must be given preventative therapy.
- All people living with HIV and AIDS have to be screened regularly. If they don’t have TB, they can be given preventative therapy to reduce their risk of contracting it.
- If someone in your house has the disease, keep your home well ventilated to prevent the spread of germs.
- Keep windows open in taxis, trains and buses to ensure good air circulation.
Some more useful tips if you have or someone you know has TB

Respiratory hygiene and cough etiquette can prevent the spread of TB. If you have to sneeze, cough or spit, you must:
- Turn your head away from people when you cough, sneeze or spit.
- Cover your mouth when you cough or sneeze.
- Try to sneeze, cough or spit into a tissue or toilet paper. Throw the used tissue or toilet paper into a bin.
- If you don’t have a tissue or toilet paper on hand, sneeze and cough into your upper arm.
- Use a tissue or toilet paper if you need to blow your nose and throw the used tissue or toilet paper into a bin.
- If you have a cough, cold or flu, cover your mouth and nose by wearing a mask or scarf when you are in enclosed or crowded spaces, for example when visiting your clinic, travelling in public transport, or in your home.
- Continuously wash your hands so that you do not transmit germs.
Even though the Western Cape has the highest TB cure rate in South Africa, the risk for new infections remains a serious challenge. More work is required to change behaviour and address misconceptions at an individual level, as well as efforts to address the challenges facing our communities.
For more information and medical advice, please go to one of your local primary healthcare clinics or TB hospitals.
TB Statistics for South Africa – National & provincial
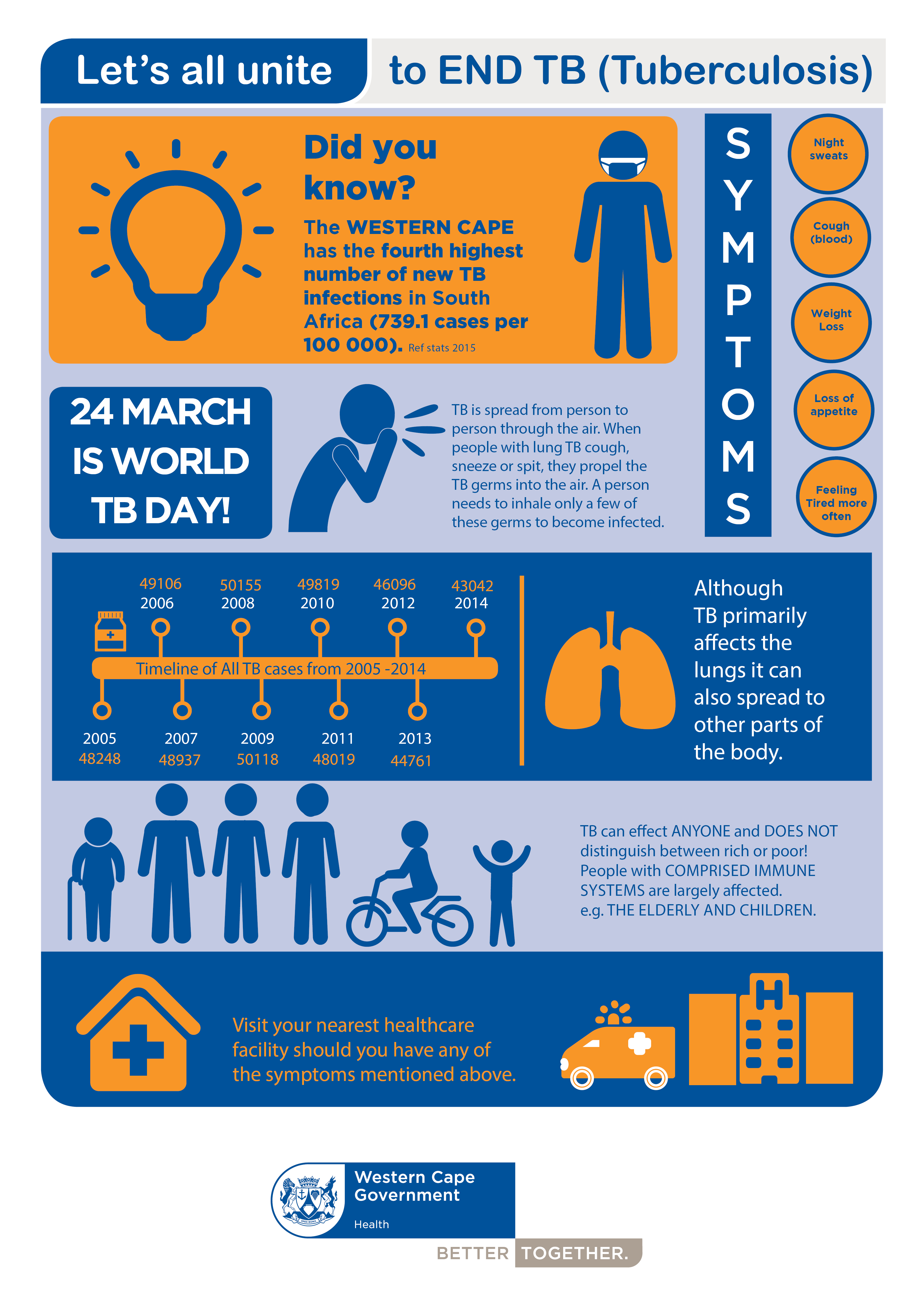 The World Health Organization (WHO) and partners are promoting dialogue and collaboration that unites individuals and communities in new ways to end the tuberculosis (TB) epidemic.
The World Health Organization (WHO) and partners are promoting dialogue and collaboration that unites individuals and communities in new ways to end the tuberculosis (TB) epidemic.
Four sub-themes under the “Unite to End TB” theme that WHO is promoting are:
- Together we will tackle TB by stamping out poverty.
- Together we will better test, treat, and cure.
- Together we will stop stigma and discrimination.
- Together we will drive research and innovation.
The aim is to ensure early diagnoses, successful treatment of tuberculosis (TB) patients and strengthening of partnerships between local and provincial health authorities and citizens, to eliminate the threat of TB in the Western Cape by working better together.
South Africa has adopted the new UNAIDS strategy aimed at bringing about an HIV free generation called the ’90 90 90’ strategy. This strategy aims to ensure that by 2020,
- 90% of all people living with HIV will know their status,
- 90% of those eligible for treatment with Anti-retroviral treatment (ART) will be on sustained treatment, and
- 90% of people on ART will have suppressed viral loads.
The ’90 90 90’ strategy has also been adapted for TB, so that by 2020,
- 90% of vulnerable groups should have been screened for TB,
- 90% of people with TB should be diagnosed and started on treatment, and
- 90% of those treated for TB should be cured.
The aim with this inclusive strategy is that no one will be left out. The increasing number of people who are infected with TB will only be manageable if those who have been diagnosed with TB complete their treatment.
Together, we can stop the spread of TB:


